Streamline attendance tracking, service billing, and reimbursement workflows with iCareManager’s integrated Attendance & Billing solution. Built for long-term care, IDD programs, HCBS providers, and assisted living agencies, iCM helps you record attendance accurately, generate clean 837 billing files, reduce errors, and accelerate Medicaid and insurance reimbursement with real-time visibility and automated data flow.

Automated Attendance Tracking
Effortlessly capture daily attendance, program hours, and service delivery with real-time, user-friendly logging - built to support HCBS, IDD, day habilitation, and long-term care programs.
Accurate 837 Billing File Generation
Automatically generate clean compliant 837P/837I billing files aligned with state and Medicaid requirements, minimizing rejections and accelerating reimbursement cycles.
Integrated Monitoring
Gain complete visibility into attendance activity, exception alerts, and billing readiness with real-time attendance monitoring designed for compliance focused agencies.
Error Reduction
Reduce manual entry mistakes and prevent billing discrepancies with automated data validation that supports audit readiness and cleaner claims.
Streamlined Reimbursement
Speed up payment processing with accurate billing data, seamless file submission, and workflows designed to improve financial accuracy and reduce claim denials.
Discover how our solution can enhance your experience with unmatched value and performance.
1
Record client attendance, program participation, check-ins, and service hours through simple, mobile-friendly interfaces, ensuring accurate data for Medicaid billing and compliance.
2
iCM automatically aggregates attendance data across sites, programs and service types, preparing clean datasets for billing calculations 837 generation, and reporting.
3
Generate fully compliant 837 billing files (837P / 837I) instantly, reducing manual prep time and ensuring submissions align with Medicaid and state billing standards.
4
Validate attendance records and billing details with built-in checks that help agencies maintain audit-ready documentation and prevent costly errors.
5
Submit billing files to payers and track reimbursement status in real time, giving your team full visibility into claims, payments, and outstanding items.
Discover how iCareManager’s Attendance & Billing solution streamlines attendance tracking, reduces billing errors, and accelerates Medicaid reimbursement for long-term care, IDD, HCBS, and assisted living programs. With real-time attendance monitoring and clean 837 billing file generation, iCM helps your team stay compliant and improve financial accuracy.
Book a Personalized Demo

Strengthen operational efficiency and financial accuracy with tools designed to streamline attendance tracking, improve billing compliance, and accelerate Medicaid reimbursement.

Reduce manual errors with automated attendance tracking and precise billing data, ensuring clean submissions every time.
.png)
Monitor attendance, service hours, and billing readiness through centralized real-time dashboards that support faster decision-making.
.png)

Accelerate Medicaid reimbursement with instant 837 file generation, fewer errors, and smoother payer submission workflows.
.png)
Stay fully prepared for compliance reviews with accurate documentation, transparent reporting, and structured billing oversight.
.png)
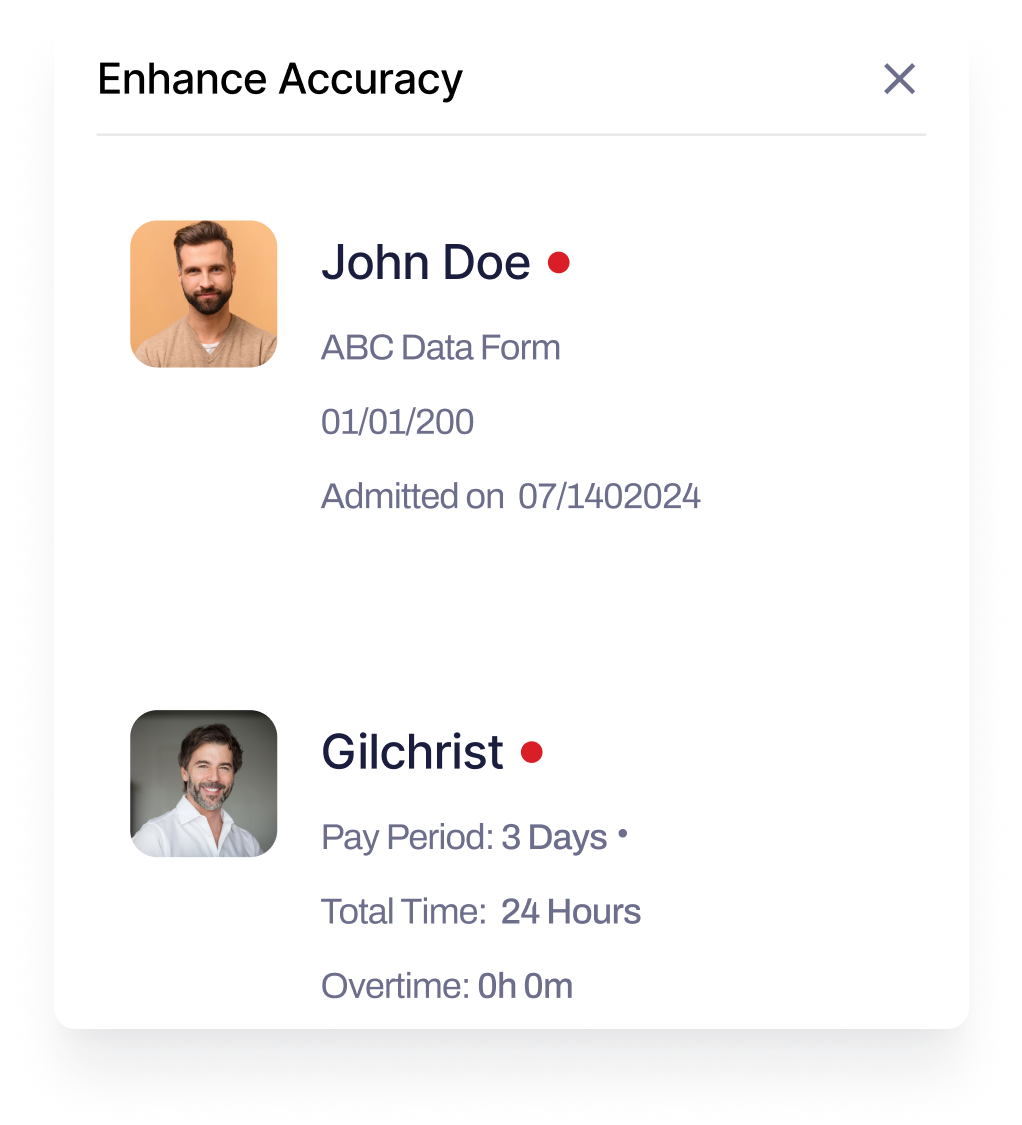
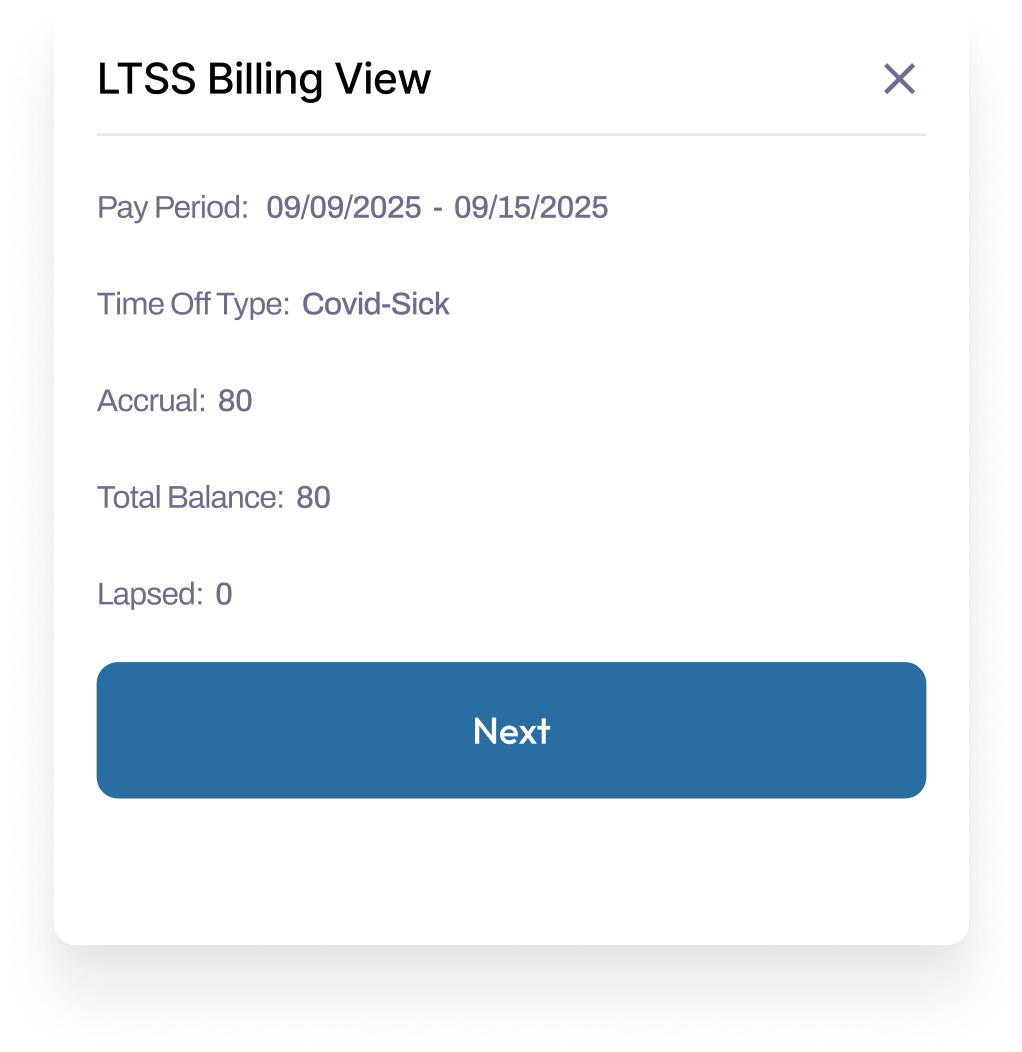
Discover additional tools that work seamlessly with the Attendance & Billing Solution to enhance accuracy, compliance and operational performance.




FAQ
Find quick answers to the most common questions about iCM’s features, support, integrations, and more.
iCM reduces errors by automating attendance tracking, validating service hours, and generating clean 837 billing files, ensuring submissions align with Medicaid and state requirements.
Yes. The Attendance & Billing solution supports IDD, HCBS, day programs, long-term care, and assisted living - capturing accurate attendance across all service models.
Absolutely. iCM provides real-time visibility into claim submission, payment status, and outstanding items, helping teams manage the reimbursement cycle more efficiently.
Yes. Automated logs, accurate attendance records, and structured billing documentation ensure your agency stays audit-ready and compliant with state and Medicaid standards.